Floaters are a common phenomenon, often described as small threads, hairs, cobwebs, or specks that drift back and forth in the vision following movements of the head or eye.
Floaters are usually the result of condensation within the gel (vitreous) in the back of the eye; these condensations develop when the vitreous separates spontaneously from the retina (the inner lining of the back wall of the eye).
Floaters are often more noticeable when one is looking at the sky or a white surface, and they are more common wit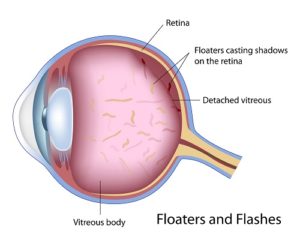 h age.
h age.
Floaters are not always a sign that there is a serious problem with the eye, but new floaters or a sudden increase in the number of floaters sometimes can be a symptom of serious conditions such as tears or detachments of the retina.
Nearsighted people can be more susceptible to these retinal problems.
Anyone experiencing new symptoms, especially a sudden shower of specks or cobwebs in the vision or flashing lights like lightning in the peripheral vision, should have a complete dilated eye examination within 24 to 48 hours by an ophthalmologist.
Shadows in the vision can be a more ominous sign of a retinal detachment, and immediate attention is required (please see Retinal Tears).
Age-related macular degeneration (ARMD) is a common condition and is the leading cause of blindness in people over the age of 60. Less commonly it can affect younger people, especially if they are very nearsighted or have had a particular type of infection in the retina.
The retina is the lining of the back wall of the eye which collects visual images and helps to transform them into visual signals that are sent to the brain.
The macula is the center of the retina and is responsible for the central portion of vision that allows us to read and see fine detail. With age, the macula of the retina can undergo degenerative changes which, if severe, can lead to serious loss of central vision.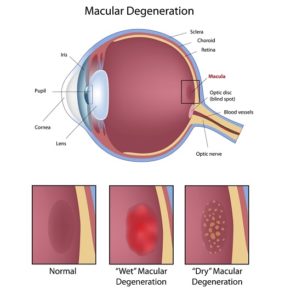
Research has indicated that genetics plays a major role in the susceptibility to macular degeneration, and a family history of ARMD in parents and siblings is a risk factor. Other risk factors include smoking, female gender, Caucasian race, and ultraviolet light exposure.
ARMD is usually divided into two categories: wet and dry.
The dry form is more common and usually affects the vision to a lesser degree. In dry ARMD, the pigment cell layer under the macula accumulates deposits of waste material, called “drusen”, which are visible to the ophthalmologist as yellowish spots in the back of the eye. Thinning and atrophy of the macula may also develop.
Often, dry macular degeneration does not affect the vision to a significant degree, but in more severe cases the vision can become blurred or blind spots or blank areas may appear in the central vision.
There is no known effective way of reversing dry macular degeneration. However, the age-related eye disease studies 1 and 2 (AREDS) have shown that specific doses of the antioxidant vitamins A, E, C, and Zinc, as well as lutein and zeaxanthin, can slow the progression of moderate and severe dry macular degeneration, thus reducing the risk of vision loss. AREDS supplements should only be taken after consultation with a medical doctor as they can have side effects.
Wet macular degeneration is so-called because it is the result of tiny abnormal new blood vessels that grow and break into space under the macula, causing leakage of blood and fluid.
It is often preceded by dry degeneration, and an exam by an ophthalmologist can identify people who may be asymptomatic but at risk for the development of this more severe form of the disease.
Wet macular degeneration is less common, but when it occurs, it often can cause a more serious loss of vision. Symptoms may begin as gradually progressive blurring or distortion of the vision.
Straight objects such as telephone poles or Venetian blinds may appear crooked. Sometimes the loss of vision occurs abruptly and with no warning.
People with this form of the disease in both eyes who are either not treated, or who do not respond well to treatment, may end up losing the ability to read, drive, or recognize faces.
Peripheral vision loss is not typical in this condition, and people with central vision loss often remain able to function independently.
However, they may require assistance with tasks involving reading, writing, cooking, and transportation.
Macular degeneration can be diagnosed by an ophthalmologist with a dilated fundus exam in the office.
Many times, another testing such as angiography (a photographic test to look at the retina involving the injection of intravenous dye) or ocular coherence tomography (a sophisticated digital imaging study of the macula) may be necessary to aid in diagnosis and to formulate the appropriate treatment as indicated.
There are no cures for dry or wet macular degeneration, but several treatments for wet macular degeneration have become available which can halt its progression and, in some cases, even reverse the loss of vision.
These treatments commonly involve the injection of medications into the eye (intravitreal injection) such as Lucentis, Avastin, or Triamcinolone. Photodynamic therapy is another treatment that is sometimes used and requires the injection of a medication called Visudyne into a vein in the arm.
Fifteen minutes after the start of the injection, a low power red light laser is used to activate the medication in the back of the eye in order to seal off leaking blood vessels under the macula. This procedure is often combined with an intravitreal injection.
Conventional laser treatment may still sometimes be employed to cauterize leaking blood vessels, but this treatment is less commonly performed now, as the newer treatments give a better prognosis for visual recovery.
Unfortunately, none of the treatments mentioned above are effective in all patients, and even when they are effective, they often need to be repeated periodically to control the disease.
There is much ongoing research regarding macular degeneration, and many experimental treatments are being tested in academic centers.
This research will certainly lead to further improvements in treatment in the future.
However, patients should always seek the opinion of an ophthalmologist prior to embarking on any “new” expensive therapies that might be seen promoted on the internet and elsewhere.
A sudden increase in floaters (drifting spots, hairs, cobwebs in the vision) with or without accompanying flashes of light, usually indicates that the vitreous gel filling the back of the eye has separated from the retina (the inner lining of the back wall of the eye).
This is known as a posterior vitreous detachment and occurs naturally, usually between the ages of 50 and 70. Most of the time, when a vitreous detachment occurs, no damage results and no treatment is required.
The symptoms may gradually subside over several weeks, although it is not unusual to have persistent floaters in the vision. In about ten percent of cases, a vitreous detachment can lead to a tear in the retina which, if not treated, can lead to a retinal detachment.
Retinal tears and detachments can affect anyone, but they are more common in nearsighted people and in those with a family history of these problems.
Retinal detachments, if not treated promptly, can lead to serious permanent loss of vision. It is imperative that a patient is seen by an ophthalmologist promptly if new floaters, flashes, or shadows develop.
If a tear is present and is diagnosed and treated quickly, retinal detachment can be prevented. When a retinal tear is discovered, it can be treated in an office setting with retinal laser or freezing treatments.
This treatment creates a scar around the tear that can prevent subsequent development of retinal detachment.
Diabetic retinopathy: Diabetes is a problem where the body loses the ability to control the amount of glucose, or sugar, in the blood. Glucose is the fuel that your brain and nervous system use to keep running, but when glucose levels are too high, small blood vessels and capillaries in all the body’s tissues become damaged.
In the eye, the tissue most susceptible to damage is the retina. The retina acts like the film in a camera; it is the thin inner lining of the back wall of the eye that is responsible for capturing the visual information that ultimately gets sent back to the brain.
The retina is very delicate and has more blood vessels in it per unit weight than any other tissue in the body.
Therefore, it is very sensitive to damage from high glucose levels, and damage to the retina, or diabetic retinopathy, eventually leads to vision loss.
A significant amount of damage may occur to the retina before vision is affected, and sometimes this damage is permanent. It is essential to prevent retinopathy or minimize retinopathy through strict control of blood sugar with diet, exercise, oral medications, and, if necessary, insulin.
Periodic dilated eye exams are also essential to enable the ophthalmologist to diagnose retinopathy at an early stage when it can be effectively treated. Waiting until the vision loss has occurred makes treatment more difficult and less effective.
Treatment for diabetic retinopathy often involves the use of lasers. Laser treatments may be directed at the macula, the central portion of the retina, in order to treat areas of swelling caused by leaking blood vessels.
If untreated, the swelling can lead to progressive vision loss. When retinal damage reaches a more severe level, new abnormal blood vessels will start to grow within the eye, which can lead to bleeding, scar tissue formation, retinal detachment, and permanent total loss of vision.
If new blood vessels or bleeding are found, a laser may be used to treat the peripheral portion of the retina in a procedure called pan-retinal photocoagulation.
This treatment is a little more intense and is often broken up into two or more sessions. The goal of this treatment is to cause abnormal vessels to shrink and stop bleeding.
Any blood that is already present, which the patient may note as floating spots in the vision, may slowly absorb on its own. However, if the bleeding is severe, surgical removal of the blood may be required.
As an alternative to laser treatment, or sometimes in conjunction with a laser, certain medications may be injected directly into the eye in a procedure called intravitreal injection.
The injected medications are often effective in shrinking new blood vessel growth and in improving macular swelling, but they may need to be repeated periodically.
If diabetic retinopathy becomes advanced, either because it is diagnosed at a late stage, or because it does not respond well to treatment, surgery in an operating room is sometimes necessary.
This usually involves removing the gel from within the eye in a procedure called a vitrectomy.
Blood and scar tissue may also be removed. Vitrectomy can be very effective in restoring vision, but at times, when retinopathy is very advanced, even surgery fails to restore vision, and blindness can occur.
Diabetic retinopathy is an example of a disease for which prevention, early diagnosis, and timely treatment make all the difference. It is vital for patients to maintain strict control over their blood sugar, blood pressure, and cholesterol by following an appropriate diet and exercise regimen and by using medications when needed.
Patients who have regular visits with their ophthalmologists and undergo appropriate treatment when indicated, ideally when vision is still excellent, are much more likely to maintain good vision throughout their lives.